For most of the history of modern biomedical research, scientists have been focussing on disease genes in order to find out what causes diseases and how we can treat them. However, as even every lay person knows, not every individual has the same susceptibility to fall ill from certain conditions. For instance, people who exercise regularly tend to be more healthy and generally less likely to fall ill. People who take cold showers tend to be less susceptible to infectious diseases. The exposure to exercise or cold somehow makes individuals able to fight back diseases more efficiently.
In her recent very insightful article “The Biology of Physiological Health”, Janelle Ayres highlights different mechanisms that could be at play to promote human health. According to her article, physiological health mechanisms can be either defensive or homeostatic in nature.
Defensive health mechanisms are mechanisms that enable an organism to either antagonize or withstand an insult. For instance, when faced with the temptations of an all-abundant high calorie diet, which is well-known to promote a myriad of diseases, we can use defensive strategies to avoid or eliminate the stressor. This may involve not eating high calorie food or engaging in a heavy exercise regimen to burn the calories and prevent fat build-up. Similarly, when faced with potentially pathogenic microorganisms, we could avoid being exposed to them or eliminate them via our immune system.
An alternative defensive health strategy is to neutralize the stressor. In the case of fat build-up, this may involve depositing the diet derived fat in subcutaneous adipose tissue (the fat below our skin, which is considered beneficial) as opposed to visceral adipose tissue (the fat in our abdominal cavity, aka belly fat, which is much more harmful). Such a health-promoting distribution of fat is physiologically mediated by estrogen in women. Therefore, the estrogen induced female type fat deposition can be considered a physiological defensive health mechanism.
Finally, organisms can also develop strategies to be able to tolerate the presence of a stress signal. For example, repeated cold exposure leads to the development of brown fat, which produces heat and helps to maintain the body temperature and avoid cold temperature related pathology. Another example are facultative pathogens, which in most individuals are tolerated and held in check by the immune system (without being eliminated).
A prime example for organisms that use a tolerance-based defensive strategy are bats. Bats have developed tolerance to many viral infections by dampening their immune response and co-existing with the viruses (
Gorbunova et al. 2020). This is one major reason why bats are an important reservoir for viral diseases that can cross over to humans.
In summary, defensive health strategies are induced in response to a stressor or pathogen and include strategies to avoid, eliminate, neutralize or tolerate the stress signal.
On the other hand,
homeostatic health mechanisms have been defined as regulatory mechanisms that help an organism to adapt to fluctuations in external or internal conditions in order to maintain a constant internal environment (
Ayres, 2020). Homeostatic health mechanisms, which are also referred to as vigor, operate constantly at the level of cells, tissues and the whole body. They ensure that cells, tissues and the organism function in a non-disturbed manner. According to Ayres, homeostatic health mechanisms require sensing mechanisms for specific variables. The sensed information is then integrated by a control center, which provides an output to restore the set point of the particular variable.
A good example for a homeostatic health mechanism that operates at the whole organism level is the leptin pathway. When there is an increase in adipose tissue mass, more of the hormone leptin will be released from the adipose tissue into the blood stream. In the hypothalamus, leptin receptors then mediate a response, resulting in decreased hunger and increased energy expenditure. As a consequence, the body weight returns to the set point. Individuals that lack an efficient response to leptin (leptin resistance) are more prone to gain weight. Individuals with a highly functional leptin pathway are likely to resist weight gain even when challenged with high calorie food.
Homeostatic health mechanisms can also operate at the tissue level, for instance in the bone regeneration process. In bone remodeling, old bone is destroyed by osteoclasts and replaced with bone that is newly formed by osteoblasts. The process of bone remodeling is required for the repair of bone damage, which occurs constantly due to physical load and muscle contraction. Bone regeneration is a good example for a homeostatic health mechanism because impairment of this process during aging leads to osteoporosis. The onset of the disease is in this instance not due to increased stress (i.e. increased load and muscle activity), but a consequence of impaired homeostasis mechanisms. The impairment in bone remodeling thus results in a lower threshold to induce a disease state.
There are many examples for homeostatic health mechanisms at the cellular level. For instance, in the endoplasmic reticulum (ER) stress response pathway, sensor chaperones such as BiP/GRP-78 continuously monitor the accumulation of unfolded proteins in the ER. Sensing of increased amounts of unfolded proteins then triggers various stress response pathways to re-establish ER homeostasis by promoting ER protein folding by chaperones, lowering the ER protein load by inhibiting the synthesis of new proteins and promoting the degradation of unfolded proteins.
Another example for a cellular homeostatic health mechanism is the DNA damage response, e.g. in our skin cells. Our skin is exposed to DNA mutation-inducing UV irradiation on a daily basis. In order to prevent that DNA mutations are passed on to daughter cells during cell division, cells activate DNA damage repair pathways and only enter mitosis when the DNA damage repair has been completed. As such, skin cancer, which often arises as a consequence of UV-induced DNA damage, can be understood as a failure of a homeostatic health mechanism.
One important distinguishing feature between defensive and homeostatic health mechanisms is that defensive mechanisms are initiated in response to a stressor or pathogen in order to prevent disease. On the other hand, homeostatic health mechanisms are continuously active and improve health, even in the absence of a specific disease-causing stressor or pathogen. Due to improved health, an organism becomes less likely to become ill. In other words, homeostatic health mechanisms increase the threshold to move an organisms from the healthy state to a disease state. Importantly, while defensive and homeostatic health mechanisms are normally present in our body, tissues and cells, they can also be induced therapeutically, for instance through medications or life style changes.
Physiological health mechanisms are very interesting concepts, which challenge the way we normally think about human health and disease. However, why is it important to understand about different health mechanisms, for instance when characterizing or devising novel treatment strategies? In other words, why is it important to know whether a therapy induces defensive strategies or improves homeostatic health meachanisms?
There are likely a number of reasons why knowing the mechanism that underlies a therapeutic intervention is useful.
Firstly, it can give information about whether a certain treatment has more narrow or broader therapeutic applications. For instance, in obesity therapy, treatments such as an increase in energy expenditure or bariatric surgery are clearly defensive therapeutic strategies that improves a disease condition, but do not make normal individuals more healthy. In fact, drugs that increase energy expenditure or bariatric surgery are likely to be detrimental to healthy individuals with normal BMI.
On the other hand, improving leptin response is a homeostatic mechanism that improves obesity but also helps to maintain a healthy fat mass and prevent weight gain, e.g. during aging. Needless to say, certain therapeutic approaches could also have both defensive and homeostatic health components. One example is exercise, which can defend the body weight in response to high calorie intake or lower the body weight in obese individuals. At the same time, exercise is well know to promote various homeostatic health mechanisms, including strengthening of the immune system, improving insulin sensitivity and conditioning of the cardiovascular system.
The examples given are rather obvious and it would be straight forward to predict whether the described interventions have defensive or homeostatic mechanisms of action.
However, if we for instance perform a genomics study for susceptibility genes in a specific disease and find a gene that potentially protects organisms from the disease, we do want to know whether the gene is involved in defensive and homeostatic mechanisms. Knowing this would for instance help with the design of experiments to characterize the role of the gene. If the gene has a defensive mechanism, we would study how the gene product prevents the onset or severity of a disease in response to specific stress signals that trigger the disease. In contrast, if the gene product promotes homeostatic health mechanisms, we would examine its role in healthy individuals and determine changes in the threshold required to develop the disease.
Furthermore, treatments that work via defensive health mechanisms are only indicated if a person is exposed to a specific risk factor for the disease or if a person has developed the disease. In contrast, treatments that work via homeostatic health mechanisms are likely applicable to a wide range of healthy individuals. Furthermore,defensive health mechanisms are more likely to be stimulus-specific, whereas homeostatic health mechanisms likely have broader, more general health effects.
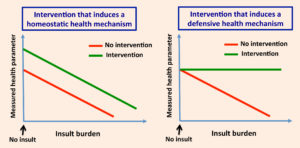
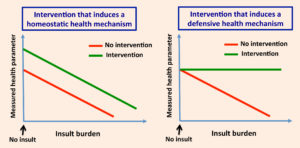
Importantly, Janelle Ayres also describes approaches how we can experimentally determine if a health intervention works via a homeostatic mechanism. One approach is to expose an organism (or potentially even cultured cells) to no treatment and increasing doses of the stress signal and then measure a parameter that is indicative of health. If the health intervention increases the health parameter at any dose of the insult and even in the absence of the insult, this would indicate a homeostatic health mechanism. As shown in the Figure below, homeostatic health interventions raise the health parameter trendline without changing the slope, thus essentially making the organism more healthy or more resistant to develop a disease. In contrast, if the health intervention works via a defensive mechanism, the decline in the health parameter with increasing insult dose is prevented. However, defensive health interventions do not affect the health parameter in the absence of the stress signal.
Many homeostatic health mechanisms likely existed in our ancestors as a natural way of life. For instance, a health intervention that promotes health span and is likely homeostatic in nature is intermittent fasting. Intermittent fasting is something that probably existed quite naturally in our ancestors due to limited and periodic food availability. In contrast, in our present-day civilization food is constantly available. Other examples include exercise, which our ancestors had to do in order to survive, or intermittent cold exposure, which may strengthen the immune system. Hence, this raises the possibility that many of the diseases in modern times are due to the loss in homeostatic health mechanisms as a result of lifestyle changes brought about by the industrialization.
On the other hand, our ancestors also spent extended periods of time sedentarily, similar to humans in the industrialized area. The negative effects of a sedentary lifestyle are in large part due to lower muscle activity. Of note, as opposed to sitting on chairs, our ancestors likely spent most of their time when resting in a squatting position. A recent study has shown that squatting involves higher levels of lower limb muscle activity than chair sitting, explaining why a sedentary lifestyle in the industrial age is so detrimental for human health.
To improve human health in the industrialized age, the ultimate goal is to create treatments (in the broadest sense, not necessarily only in the form of medication) that work via homeostatic health mechanisms. This is because defensive health strategies usually come at a cost. A prolonged inflammatory response can induce tissue damage and cancer. Killing of microorganisms often has collateral damaging effects. Many treatments that promote defensive health strategies also have side effects. In contrast, homeostatic health mechanisms improve general health. Given that they operate in healthy individuals, they are less likely to be associated with a cost. Hence, finding approaches to activate homeostatic health mechanisms is likely to improve human quality of life as well as reduce health care costs.